Cardiac Arrhythmias
 An arrhythmia, or heart rhythm disturbance, is any electrical disturbance that can occur in the heart, originating from either the upper atria or lower ventricles. Arrhythmias can be:\
An arrhythmia, or heart rhythm disturbance, is any electrical disturbance that can occur in the heart, originating from either the upper atria or lower ventricles. Arrhythmias can be:\
- Bradyarrhythmias (slow heart rhythms) ,or
- Tachyarrhythmias (fast heart rhythms). These are subdivided into supraventricular(arising from above the ventricles, that is the atria) or ventricular (arising from either of the bottom ventricles)
Your physician will assess your symptoms and attempt to capture this arrhythmia with an electrocardiogram (EKG) monitoring modality, including a Holter or Event monitor and a 12-lead EKG. If you have persistent symptoms despite medications, or an unclear diagnosis after an extensive workup for a symptomatic arrhythmia, your physician may refer you to a heart rhythm specialist for an electrophysiology study and possible catheter ablation.
Bradyarrhythmias
Bradyarrhythmias, by definition, are slow heart rhythms, typically less than 60 beats per minute. Bradyarrhythmias can be asymptomatic, or symptomatic, related to the resultant slow heart rhythm. Sometimes both fast and slow heart rhythms coexist, leading to a condition known as tachycardia-bradycardia (tachy-brady) syndrome. Tachycardia, the opposite of bradycardia, reflects a fast heart rhythm, typically greater than 100 beats per minute.
As described earlier, the sinus node, a structure in the high right atrium, depolarizes typically 60 to 90 times per minute sending a sinus electrical impulse throughout both atria to the AV node. In brief, this leads to synchronized biatrial contraction before ventricular contraction forces blood out of the heart into the circulation. The AV node, a structure that sits in the middle of the heart, is normally the only electrical connection between the atria and the ventricles. The AV node serves as a traffic signal, controlling the rate of electrical impulses from the atria allowed to reach the ventricles, limiting the danger of 1 to 1 conduction of fast rhythms from the atrium to the ventricles. The electrical impulse that travels through the AV node eventually travels via a specialized network of fibers, known as the left and right bundle branches, to ultimately enter the ventricular muscle at its terminal ends, the Purkinje fibers.
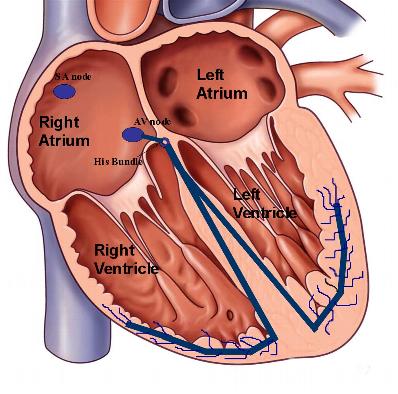 Figure 1. Illustration of the normal conduction system. The sinus node, located in the high right atrium depolarizes and sends an electrical impulse through both atrium typically at a frequency of 60 – 90 beats per minute. In order for this impulse to reach the ventricles in normal hearts, it must traverse the AV node where it encounters a normal minimal delay before it continues its path to the ventricles via the bundle branches.
Figure 1. Illustration of the normal conduction system. The sinus node, located in the high right atrium depolarizes and sends an electrical impulse through both atrium typically at a frequency of 60 – 90 beats per minute. In order for this impulse to reach the ventricles in normal hearts, it must traverse the AV node where it encounters a normal minimal delay before it continues its path to the ventricles via the bundle branches.
A slow heart rate, or bradycardia (less than 60 beats per minute), does not necessarily imply a cardiac rhythm problem. Many individuals can have a slow sinus rhythm, known as sinus bradycardia, at baseline or at times of rest, including sleep. Professional athletes or physically active persons can frequently have resting heart rates in the 40 beats per minute range. If this bradycardia is symptomatic or inappropriately slow for the conditions (i.e, during exercise or stress), it likely represents a pathologic process, or a bradyarrhythmia. We will be covering two of the most common bradyarrhythmias:
Tachyarrhythmias
Supraventricular tachycardia (SVT)
Supraventricular tachycardia, or SVT, refers to fast heart rhythms that originate from above the ventricles, hence the term. Typically physicians consider heart rates above 100 beats per minute as rapid, and classify them as tachycardia. Palpitations can be a physical symptom that patients experience secondary to an SVT, but it is not specific to SVTs. Palpitations can be caused by extra beats from either the lower (ventricular) or upper heart chambers (atria), and not necessarily from sustained fast rhythms, or tachycardias. These palpitations can last from seconds to hours. Supraventricular tachycardias are generally not life-threatening, but their symptoms can be dehabilitating to patients.
Other symptoms experienced during an episode of SVT include dizziness, shortness of breath, chest pain, and light-headedness. Patients may report these symptoms worsening with exercise, anxiety, or caffeine ingestion. Loss of consciousness, or syncope, is rarely due to an SVT, and it necessarily implies seeking prompt medical attention. Occasionally patients may not experience any symptoms during an episode of SVT. Your physician can diagnose and differentiate an SVT from other rapid heart rhythms via an electrocardiogram (EKG) obtained during the episode. However, many patients have their episodes outside their physician’s office or hospital. In these situations 24-hour Holter monitors or event monitors can be useful to catch the event.
Medications can be used to treat many patients with SVT. These medications are dictated by the type of SVT and the coexisting medical conditions patients may have. The most common class of medications for SVT include:
- Beta-blockers
- Calcium channel blockers
- Antiarrhythmic agents
Medications for the treatment of SVT can act to slow conduction from the top atria to the lower ventricles by decreasing conduction at the AV node (including b-blockers and calcium channel blockers) or by acting directly on the atrial or ventricular tissue (as with antiarrhythmics). A special procedure, called an electrophysiology study (EPS) and radiofrequency ablation (RFA)can be an alternative to medication to treat many patients who are either intolerant of medication side effects or who have recurrent symptomatic breakthrough episodes on medications.
Supraventricular tachycardias are typically classified by their origin and mechanism of perpetuation. In general terms, an SVT is due to either a reentrant circuit (continuous loop) or a focal firing of irritable tissue. A reentrant circuit is sustained by tracts of heart muscle cells that allow an electrical impulse to self-perpetuate in an endless loop.
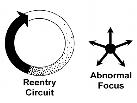 Figure 2. Depiction of a reentry circuit mechanism of tachycardia versus an abnormal focus. In a reentry circuit, the electrical impulse travels in a loop of excitable tissue, self-perpetuating the rhythm disturbance. In a focal tachycardia, a particular site of myocardial tissue abnormally fires at a rate typically faster than the sinus node, suppressing the normal mechanism of cardiac depolarization.
Figure 2. Depiction of a reentry circuit mechanism of tachycardia versus an abnormal focus. In a reentry circuit, the electrical impulse travels in a loop of excitable tissue, self-perpetuating the rhythm disturbance. In a focal tachycardia, a particular site of myocardial tissue abnormally fires at a rate typically faster than the sinus node, suppressing the normal mechanism of cardiac depolarization.
We will discuss the following SVTs in further depth:
- Atrial tachycardia
- AV nodal tachycardia (AVNRT)
- Atrioventricular tachycardia (AVRT) secondary to accessory pathway, WPW syndrome
- Atrial flutter
- Atrial fibrillation
Ventricular Tachyarrhythmias
Ventricular tachyarrhythmia is a term designated to those tachycardias, or fast heart rhythms, that originate from the lower ventricles. These rhythm disturbances are varied, most often linked to structural heart disease with or without coronary artery disease. Ventricular tachycardias are potentially the most dangerous heart rhythm disturbances, requiring the most aggressive therapy.
Patients with heart failure and structural heart disease have a decreased heart pumping function and reduced “ejection fraction”. This means the lower ventricles, typically the left ventricle, is either thickened or dilated, with decreased contractile function. This dilatation and enlargement of the left ventricle can lead to areas of fibrosis and replacement of muscle tissue with scarring. As well, coronary artery disease itself, with a history of myocardial infarctions, or “heart attacks”, leads to scarring of the heart with dilatation and segmental areas of poor contraction. This scarring and dilatation of the left ventricle can lead to the initiation and perpetuation of ventricular tachycardia (VT).
Ventricular tachycardia can originate from the left or right ventricle, with left ventricular tachycardia more common in those patients with heart failure and coronary artery disease. Ventricular tachycardia encompasses all fast heart rhythms, typically >100 beats per minute, originating from the ventricles. It can be regular, with one repetitive form or morphology, also known as monomorphic VT. If it is fast and irregular, with beat-to-beat variations, it is known as polymorphic VT. Ventricular tachycardia in patients with structural heart disease is typically due to a “reentry” mechanism, where the electrical current travels in a loop of tissue that is scarred with slowed electrical conduction. This allows the rhythm to continually perpetuate itself, as the head of the myocardial electrical current chases its tail.
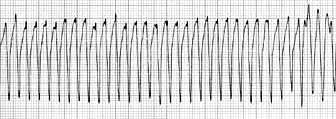
Figure 3. An EKG strip of monomorphic VT with a regular, repetitive wide-based rhythm.
A prolonged episode of sustained ventricular tachycardia can lead to sudden cardiac arrest and ventricular fibrillation (VF). Ventricular fibrillation is represented by “chaotic” ventricular activity, greater than 250 beats/min, with essentially no organized ventricular activity and resultant hemodynamic collapse. There are many causes of VF, beyond the scope of this discussion.
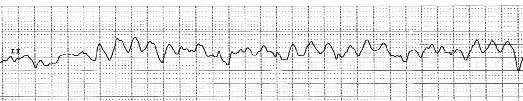
Figure 4. An EKG strip of ventricular fibrillation, with disorganized, chaotic ventricular activity.
Ventricular tachycardia can also occur in patients with structurally normal hearts, unrelated to any history of coronary artery disease. It can occur in both the young and the old, and can be a benign, potentially treatable and curable condition. Unlike ventricular tachycardia due to coronary artery disease with scarring or a dilated left ventricle, these types of VT are typically caused by a “focal” mechanisms. In other words, there is no “reentry” loop necessary to initiate or perpetuate the rhythm, but rather a “focal” site of irritable ventricular tissue that fires faster than the normal sinus node pacemaker to lead to a wide-complex rhythm on the EKG. Ventricular tachycardia in this situation can be treated with medications, with typically significant reductions in their frequency and duration. However, some patients do fail medication therapy and can be amenable to a “curative” catheter ablation procedure.
These ventricular tachyarrhythmias will be discussed in the following sections:





 Silver Spring Office
Silver Spring Office  DC Office (at Providence Hospital)
DC Office (at Providence Hospital)  Hagerstown Office
Hagerstown Office