Electrophysiology Study (EP study)
 An electrophysiology study is a procedure performed to study the electrical system of your heart. As described in the “Normal Heart” section, the sinus node, located in the top right atrium, fires an average of 60-90 times per minute. This electrical impulse leads to bi-atrial contraction and traverses the conduction system to the AV node, where it continues its course to the ventricles to lead to their synchronized contraction, with a resultant single heartbeat and ejection of blood to the rest of the body.
An electrophysiology study is a procedure performed to study the electrical system of your heart. As described in the “Normal Heart” section, the sinus node, located in the top right atrium, fires an average of 60-90 times per minute. This electrical impulse leads to bi-atrial contraction and traverses the conduction system to the AV node, where it continues its course to the ventricles to lead to their synchronized contraction, with a resultant single heartbeat and ejection of blood to the rest of the body.
As described earlier, an arrhythmia, or heart rhythm disturbance, is any electrical disturbance that can occur in the heart, originating from either the upper atria or lower ventricles. This arrhythmiacan be a bradyarrhythmia (slow heart rhythm) or tachyarrhythmia (fast heart rhythm). Your physician will assess your symptoms and attempt to capture this arrhythmia with an EKG monitoring modality, including a Holter or Event monitor and 12-lead EKG. If you have persistent symptoms despite medications, or an unclear diagnosis after an extensive workup for a symptomatic arrhythmia, your physician may refer you to a heart rhythm specialist for an electrophysiology study.
Who benefits from an EP study?
As previously described, many arrhythmias are transient and difficult to capture in the hospital or your physician’s office with a 12-lead EKG. Outpatient ambulatory monitoring techniques including Holter and Event monitors, can increase the chances of capturing an EKG strip of the arrhythmia for further clarification. However, in many patients the arrhythmia proves elusive and they are referred for an EP study.
Other patients have clearly documented arrhythmias and elect, or are referred for, an EP study in the following situations:
- symptomatic arrhythmias despite medications
- intolerance of medications (side effects) and prefer a curative catheter ablation
- prefer a curative catheter ablation first-line to avoid medications, or secondary to occupational risks (pilots, public servants – police, fireman, etc)
- risk stratification for sudden cardiac death in the presence of structural heart disease or clinically documented arrhythmias (to determine a need for an ICD)
- assess the need for a permanent pacemaker
Pre-Procedure Instructions
The day of the study, you will be asked to arrive to the hospital early in the morning, in a fasting state, with nothing to eat after the previous midnight. Your physician may also instruct you to discontinue certain medications (b-blockers, calcium channel blockers, or antiarrhythmic medications) before the procedure. As well, you may need to have blood tests drawn several days before the procedure. Please consult with your physician if you are on coumadin or take insulin for diabetes. You will need to have someone drive you to the hospital and home after the procedure since you will be receiving sedation and will need to rest the affected leg or groin.
How is the procedure performed?
You will be brought to a special EP laboratory room and prepped with continuous monitoring devices that assess your blood pressure, pulse, EKG, and oxygen saturation throughout the procedure. As a safety precaution, a pair of large defibrillation pads will be placed on your back and chest and connected to an external cardiac defibrillator. It is rare to have to use the defibrillatorduring the procedure, but patient safety is paramount.
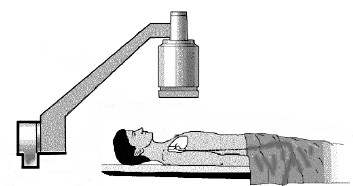
Figure 1. Illustration of the EP lab table the day of the procedure.
Thereafter, your physician and nurses will administer intravenous sedation to help you to relax during the procedure (also known as conscious sedation). After infusing a local anesthetic (numbing) medication and sterilizing your groin, your heart rhythm specialist will place several catheters, typically via the groin or neck, into the heart under fluoroscopic, or X-ray, guidance. These catheters are placed in well-defined regions critical to the heart’s normal conduction system, such as the right atrium, His bundle, and the right ventricle.

Figure 2. Image of a typical ablation catheter with a distal tip consisting of electrodes that can measure the electrical activity in the heart as well as deliver radiofrequency, or heat, energy to ablate cardiac arrhythmias.
In addition to allowing your heart rhythm specialist to measure the electrical activity in your heart, these intracardiac catheters will also allow him/her to perform pacing maneuvers in different cardiac chambers in an attempt to stimulate or elicit your clinical cardiac arrhythmia. If this is successful, your physician can electrically map the origin and mechanism of the arrhythmia.

Figure 3. Illustration of a typical EP study with catheters positioned typically near the SA node, the AV node/His Bundle, and the right ventricle. By performing pacing maneuvers with the catheters in position, your physician can determine if you have any evidence of conduction system disease. As well, your heart rhythm specialist can use the electrical signals obtained from these catheters to determine the origin of your arrhythmias during an EP study.
Although more invasive than an electrocardiogram or an ambulatory monitoring device, the EP study has the potential to provide information key to diagnosing and treating your arrhythmia. It can also be used to evaluate the effectiveness of certain medications in controlling your arrhythmia and assess your need for an implantable device (either a pacemaker or defibrillator).
Once your arrhythmia is diagnosed in the EP lab, your heart rhythm specialist can elect to proceed with a curative catheter ablation, defer to manage with medications, or recommend that you proceed with an implantable device (pacemaker or defibrillator). Before the procedure, your heart rhythm specialist will discuss your treatment options as they relate to your specific clinical arrhythmia. Not all arrhythmias can be cured with catheter ablation. Medical management or implantation of an ICD system may be recommended.
Post-procedure, what to expect
Your recovery post-procedure is generally uneventful. The catheters are removed after the procedure, typically in the EP lab. You will be transferred to the hospital recovery area where you will be monitored until you are fully awake and chatting with your family and physician. You will typically be instructed to maintain your leg straight for at least 4-6 hours after the catheters are removed to limit the possibility of developing any bleeding from the catheter site and to allow for the incision site to heal. You will typically be allowed to go home the day of an uncomplicated EP study. If you undergo a curative catheter ablation or a device implant during the same procedural day, you will likely need to plan to stay overnight in the hospital for further observation.
Complications
Complications from an EP study are minimal. Your physician will discuss with you the following possible procedure-related complications:
- bleeding or local hematoma
- infection
- damage to the artery or veins at the site of the catheter placement
- damage to the heart or vascular structures requiring surgery or implantation of a pacemaker
- lung damage
- blood clots in the veins
- stroke, MI, or death
These risks are cumulatively typically 1% or less. Your heart rhythm specialist will review these risks with you in-depth on the day of your procedure.
Discharge instructions and care
Your heart rhythm specialist will discuss specific individualized recommendations in regard to your discharge care. The following are general recommendations:
- Limit heavy lifting or strenuous exertion for 4-5 days after your study
- You may shower after your return home the day of the procedure
- You may remove any dressing or bandages placed at the catheter site after you return home
- You may typically return to work in 1-2 days, as long as it does not involve heavy lifting or strenuous exertion
- Call your physician if your incision site (typically in the groin) appears to swell or become more painful
- It is normal to develop some bruising at the catheter site with a transition to a “black-and-blue appearance” – however, this should not become more painful or lead to increased swelling after arriving home
- Follow-up with your physician in approximately 1 month for a clinic visit





 Silver Spring Office
Silver Spring Office  DC Office (at Providence Hospital)
DC Office (at Providence Hospital)  Hagerstown Office
Hagerstown Office